Не секрет, что в мире существует много болезней, которые могут годами, скрыто протекать, разрушая организм человека и становясь причиной ухудшения качества жизни человека и даже смерти. Именно одной из таких болезней, а точнее диабету посвящена данная презентация. Презентация выполнена на английском языке, хотя в рисунках и схемах содержится информация на русском языке. Данную презентацию можно использовать как на уроке по медицинской тематике, так и в качестве внеклассного мероприятия в старших классах общеобразовательных школ или в учреждениях среднего профессионального образования.
Презентация построена на общеизвестных и не совсем известных фактах относительно диабета. В презентации рассказывается о самой болезни, её причинах, её симптомах, течении, лечении, осложнениях, об образе жизни человека после обнаружения диабета, мерах профилактики, а также приводятся статистические данные по этой болезни. Благодаря презентации происходит знакомство учеников не только с этой болезнью, но и с новой лексикой, а также с техникой перевода научно-популярных статей. В презентации используется анимационный ролик на английском языке, для тренировки учеников в аудировании незнакомого материала, озвученного непосредственно носителями языка.
Diabetes, how то live with it?
Diabetes is a chronic condition associated with abnormally high levels of sugar (glucose) in the blood. Insulin produced by the pancreas lowers blood glucose. Absence or insufficient production of insulin causes diabetes. The two types of diabetes are referred to as type 1 and type 2. Former names for these conditions were insulin-dependent and non-insulin-dependent diabetes, or juvenile onset and adult onset diabetes.
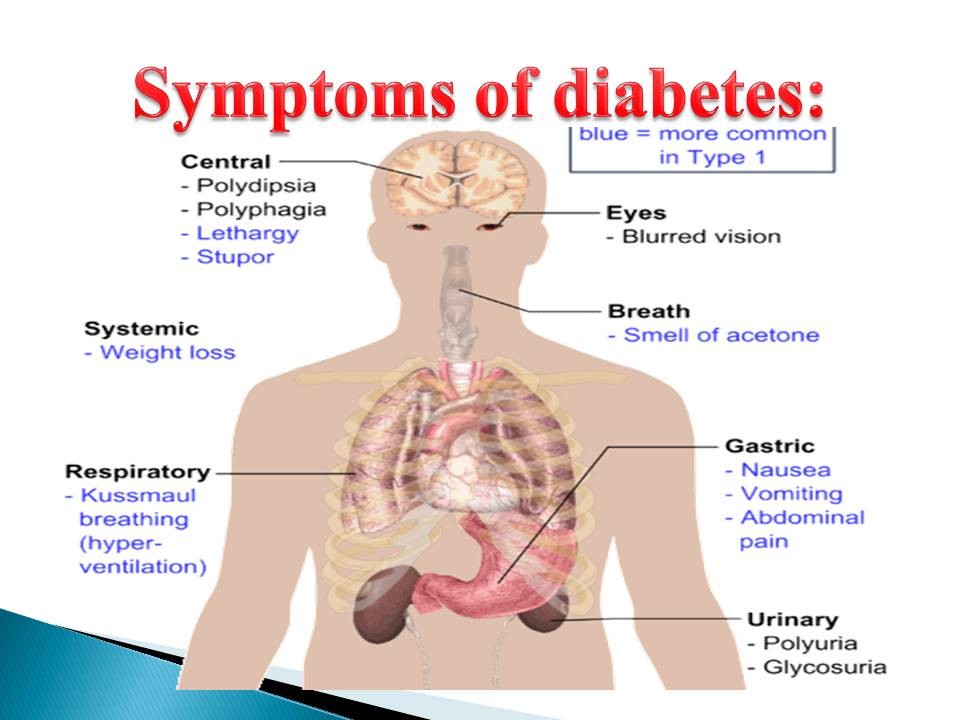
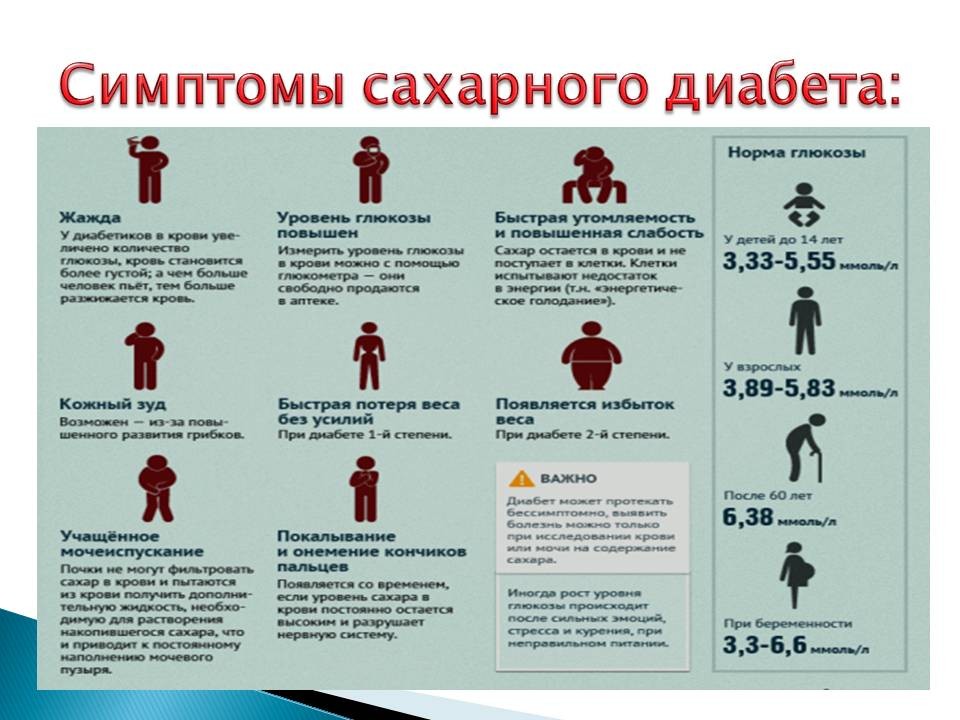
Symptoms of diabetes include increased urine output, thirst, hunger and fatigue. Diabetes is diagnosed by blood sugar (glucose) testing.
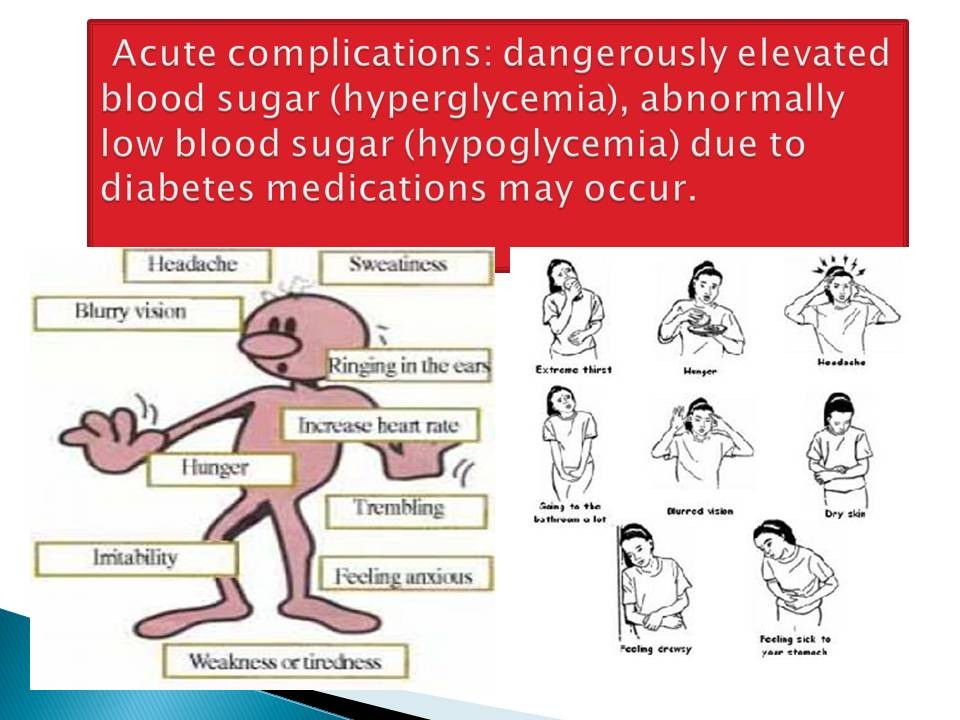
The major complications of diabetes are both acute and chronic. Acute complications: dangerously elevated blood sugar (hyperglycemia), abnormally low blood sugar (hypoglycemia) due to diabetes medications may occur. Chronic complications: disease of the blood vessels (both small and large) which can damage the feet, eyes, kidneys, nerves, and heart may occur. Diabetes treatment depends on the type and severity of the diabetes.
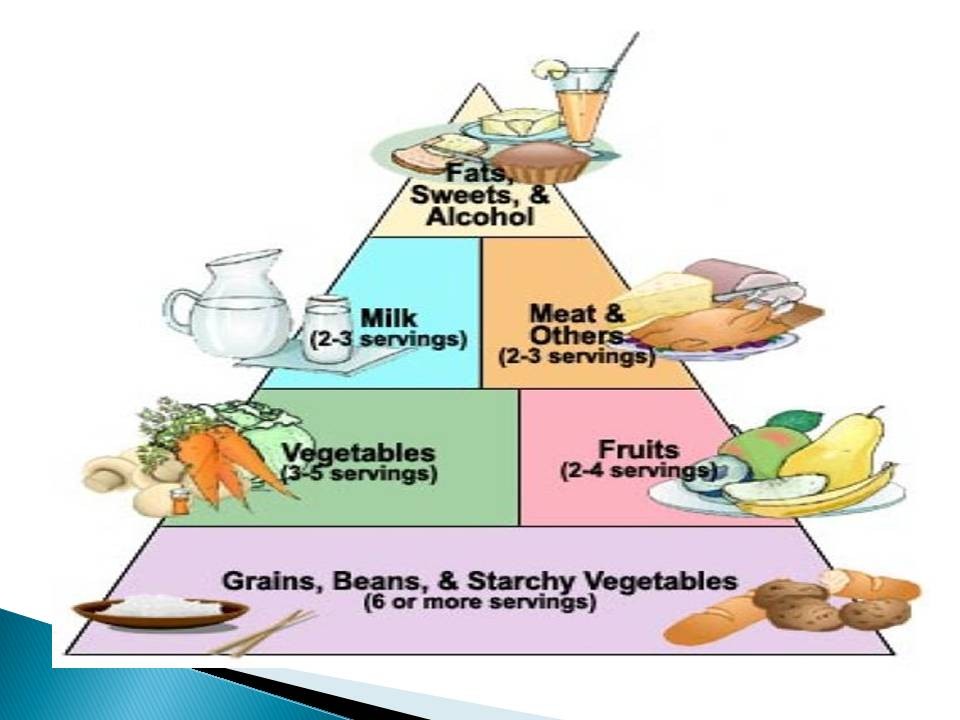
Type 1 diabetes is treated with insulin, exercise, and a diabetic diet. Type 2 diabetes is first treated with weight reduction, a diabetic diet, and exercise.
When these measures fail to control the elevated blood sugars, oral medications are used.
If oral medications are still insufficient, insulin medications and other injectables medications are considered. What is diabetes? Diabetes mellitus is a group of metabolic diseases characterized by high blood sugar (glucose) levels that result from defects in insulin secretion, or its action, or both. Diabetes mellitus, commonly referred to as diabetes was first identified as a disease associated with "sweet urine," and excessive muscle loss in the ancient world.
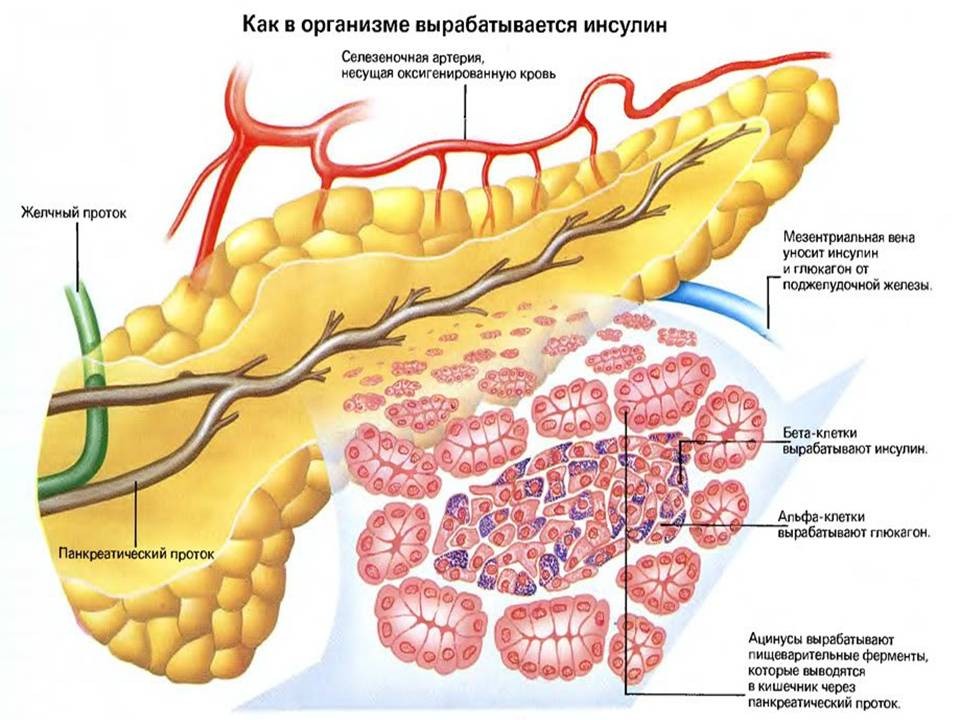
Elevated levels of blood glucose (hyperglycemia) lead to spillage of glucose into the urine, hence the term sweet urine. Normally, blood glucose levels are tightly controlled by insulin, a hormone produced by the pancreas. Insulin lowers the blood glucose level. When the blood glucose elevates (for example, after eating food), insulin is released from the pancreas to normalize the glucose level. In patients with diabetes, the absence or insufficient production of insulin causes hyperglycemia. Diabetes is a chronic medical condition, meaning that although it can be controlled, it lasts a lifetime. Over time, diabetes can lead to blindness, kidney failure, and nerve damage.
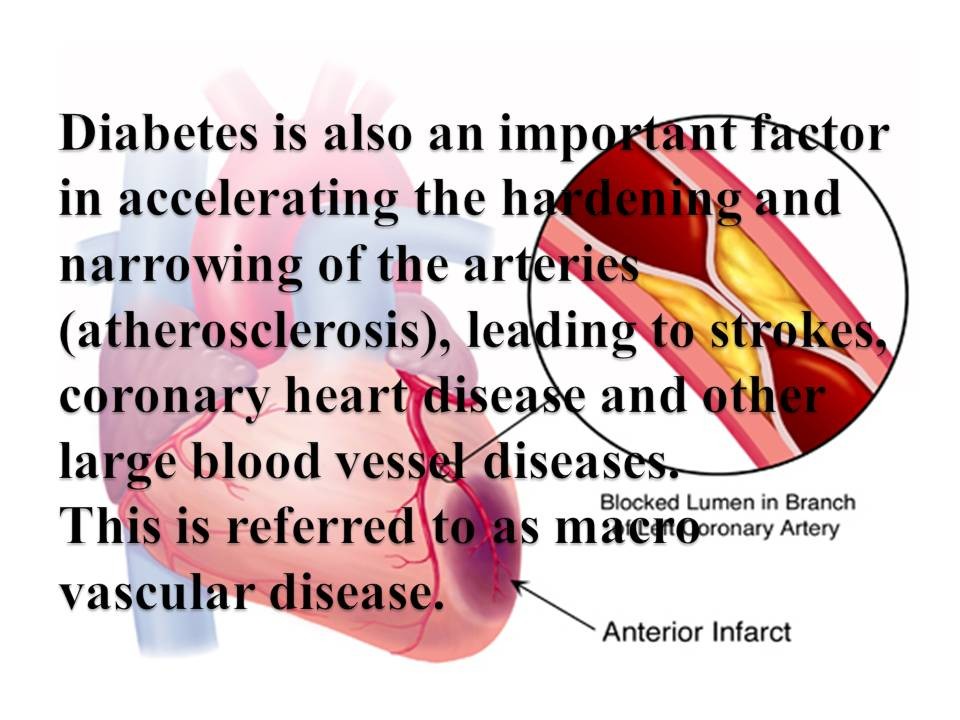
These types of damage are the result of damage to small vessels, referred to as micro vascular disease. Diabetes is also an important factor in accelerating the hardening and narrowing of the arteries (atherosclerosis), leading to strokes, coronary heart disease and other large blood vessel diseases.
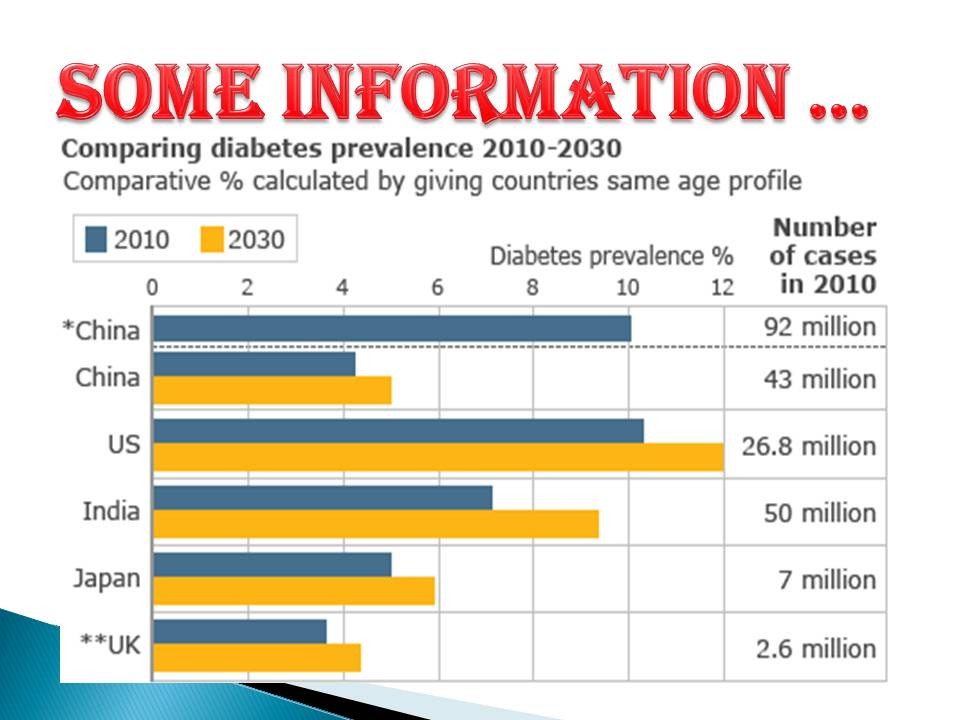
This is referred to as macro vascular disease. Diabetes affects approximately 26 million people in the United States, while another 79 million gave prediabetes. In addition, an estimated additional 7 million people in the United States have diabetes and don't even know it. From an economic perspective, the total annual cost of diabetes in 2011 was estimated to be 174 billion dollars in the United States. This included 116 billion in direct medical costs (healthcare costs) for people with diabetes and another 58 billion in other costs due to disability, premature death, or work loss. Medical expenses for people with diabetes ate over two times higher than those for people who do not have diabetes. Remember, these numbers reflect only the population in the United States. Globally, the statistics are staggering.
Diabetes was the 7th leading cause of death in the United States listed on death certificates in 2011. Insufficient production of insulin, production of defective insulin or the inability of cells to use insulin properly and efficiently leads to hyperglycemia and diabetes.
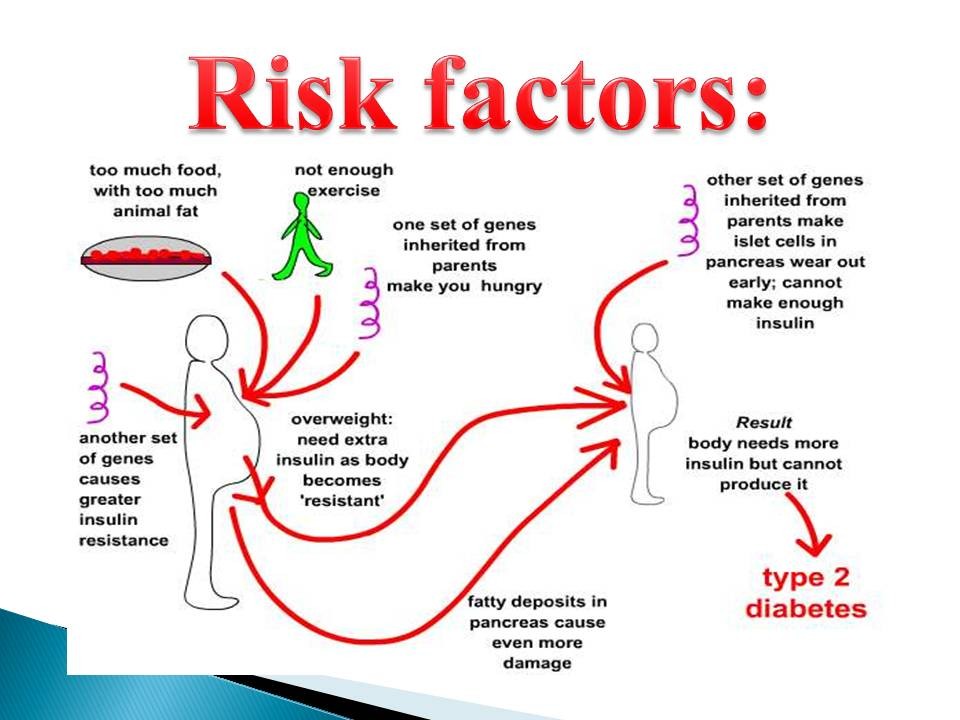
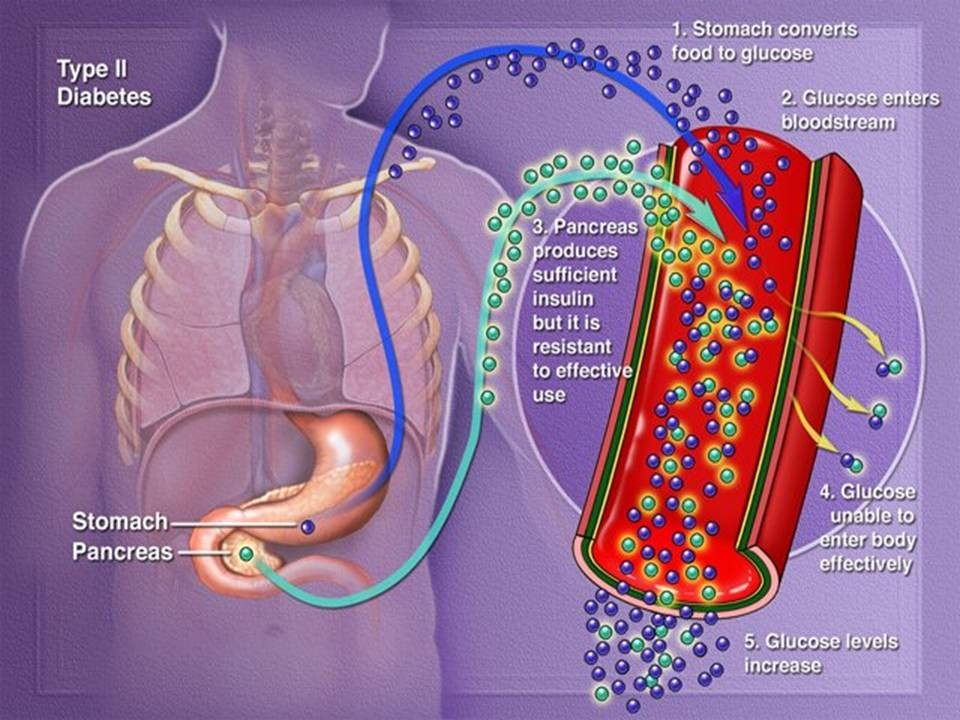
This latter condition affects mostly the cells of muscle and fat tissues, and results in a condition known as insulin resistance. This is the primary problem in type 2 diabetes. The absolute lack of insulin, usually secondary to a destructive process affecting the insulin-producing beta cells in the pancreas, is the main disorder in type 1 diabetes.
In type 2 diabetes, there also is a steady decline of beta cells that adds to the process of elevated blood sugars. Essentially, if someone is resistant to insulin, the body can, to some degree, increase production of insulin and overcome the level of resistance. After time, if production decreases and insulin cannot be released as vigorously, hyperglycemia develops. Glucose is a simple sugar found in food. Glucose is an essential nutrient that provides energy for the proper functioning of the body cells. Carbohydrates are broken down in the small intestine and the glucose in digested food is then absorbed by the intestinal cells into the bloodstream and is carried by the bloodstream to all the cells in the body where it is utilized.
However, glucose can not enter the cells alone and needs insulin to aid in its transport into the cells. Without insulin, the cells become starved of glucose energy despite the presence of abundant glucose in the bloodstream. In certain types of diabetes, the cells' inability to utilize glucose gives rise to the ironic situation of "starvation in the midst of plenty".
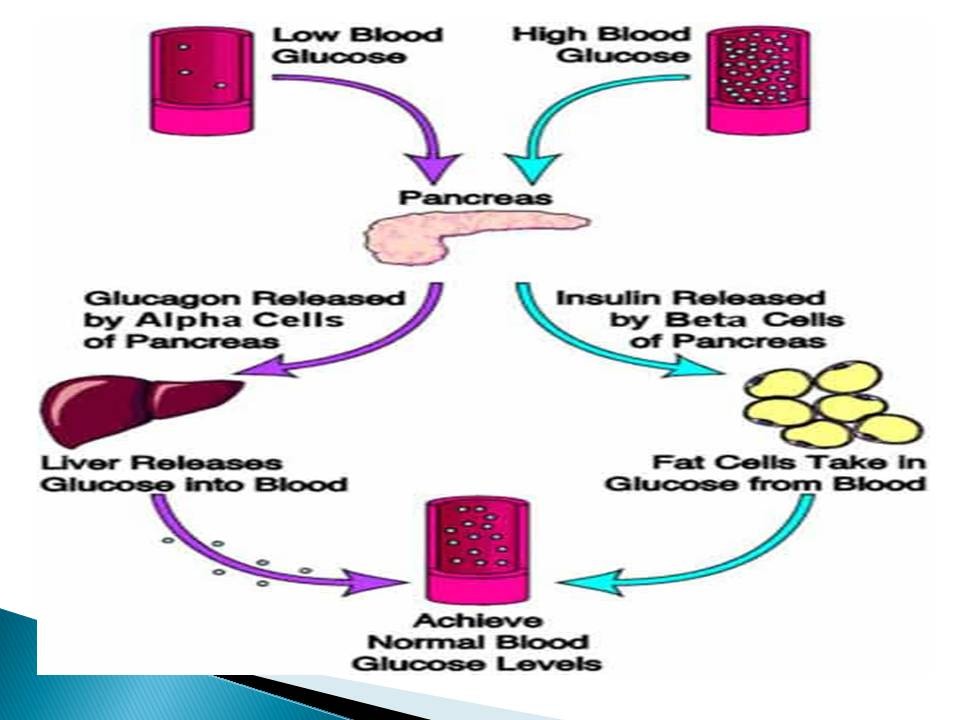
The abundant, unutilized glucose is wastefully excreted in the urine. Insulin is a hormone that is produced by specialized cells (beta cells) of the pancreas. In addition to helping glucose enter the cells, insulin is also important in tightly regulating the level of glucose in the blood. After a meal, the blood glucose level rises. In response to the increased glucose level, the pancreas normally releases more insulin into the bloodstream to help glucose enter the cells and lower blood glucose levels after a meal. When the blood glucose levels are lowered, the insulin release from the pancreas is turned down. It is important to note that even in the fasting state there is a low steady release of insulin than fluctuates a bit and helps to maintain a steady blood sugar level during fasting. In normal individuals, such a regulatory system helps to keep blood glucose levels in a tightly controlled range. As outlined above, in patients with diabetes, the insulin is either absent, relatively insufficient for the body's needs or not used properly by the body.
All of these factors cause elevated levels of blood glucose (hyperglycemia). There are two major types of diabetes, called type 1 and type 2. Type 1 diabetes was also formerly called insulin dependent diabetes mellitus (IDDM) or juvenile onset diabetes mellitus. In type 1 diabetes, the pancreas undergoes an autoimmune attack by the body itself and is rendered incapable of making insulin. Abnormal antibodies have been found in the majority of patients with type 1 diabetes. Antibodies are proteins in the blood that are part of the body's immune system.
The patient with type 1 diabetes must rely on insulin medication for survival. Exposure to certain viral infections (mumps and Coxsackie viruses) or other environmental toxins may serve to trigger abnormal antibody responses that cause damage to the pancreas cells where insulin is made. Some of the antibodies seen in type 1 diabetes include anti-islet cell antibodies, anti-insulin antibodies and antiglutamic decarboxylase antibodies.
These antibodies can be detected in the majority of patients and may help determine which individuals are at risk for developing type 1 diabetes. At present, the American Diabetes Association does not recommend general screening of the population for type 1 diabetes, though screening of high risk individuals, such as those with a first degree relative (sibling or parent) with type 1 diabetes should be encouraged.
Type 1 diabetes tends to occur in young, lean individuals, usually before 30 years of age, however, older patients do present with this form of diabetes on occasion. This subgroup is referred to as latent autoimmune diabetes in adults (LADA). LADA is a slow, progressive form of type 1 diabetes. The fasting blood glucose (sugar) test is the preferred way to diagnose diabetes. It is easy to perform and convenient. After the person has fasted overnight (at least 8 hours), a single sample of blood is drawn and sent to the laboratory for analysis. This can also be done accurately in a doctor's office using a glucose meter. Normal fasting plasma glucose levels are less than 100 milligrams per deciliter (mg/dl). Fasting plasma glucose levels of more than 126 mg/dl on two or more tests on different days indicate diabetes. A random blood glucose test can also be used to diagnose diabetes. A blood glucose level of 200 mg/dl or higher indicates diabetes. When fasting blood glucose stays above 100mg/dl, but in the range of 100-126mg/dl, this is known as impaired fasting glucose (IFG). While patients with IFG do not have the diagnosis of diabetes, this condition carries with it its own risks and concerns, and is addressed elsewhere. For the test to give reliable results: The person must be in good health (not have any other illnesses, not even a cold). The person should be normally active (not lying down, for example, as an inpatient in a hospital). The person should not be taking medicines that could affect the blood glucose. The morning of the test, the person should not smoke or drink coffee.
A person has diabetes when two diagnostic tests done on different days show that the blood glucose level is high. A pregnant woman has gestational diabetes when she has any two of the following: fasting plasma glucose of 92 mg/dl or more, a 1-hour glucose level of 180 mg/dl or more, or a 2-hour glucose level of 153 mg/dl, or more.
Home blood sugar (glucose) testing is an important part of controlling blood sugar.
One important goal of diabetes treatment is to keep the blood glucose levels near the normal range of 70 to 120 mg/dl before meals and under 140 mg/dl at two hours after eating.
Blood glucose levels are usually tested before and after meals, and at bedtime.
The blood sugar level is typically determined by pricking a fingertip with a lancing device and applying the blood to a glucose meter, which reads the value. There are many meters on the market, for example, Accu-Check Advantage, One Touch Ultra, Sure Step and Freestyle.
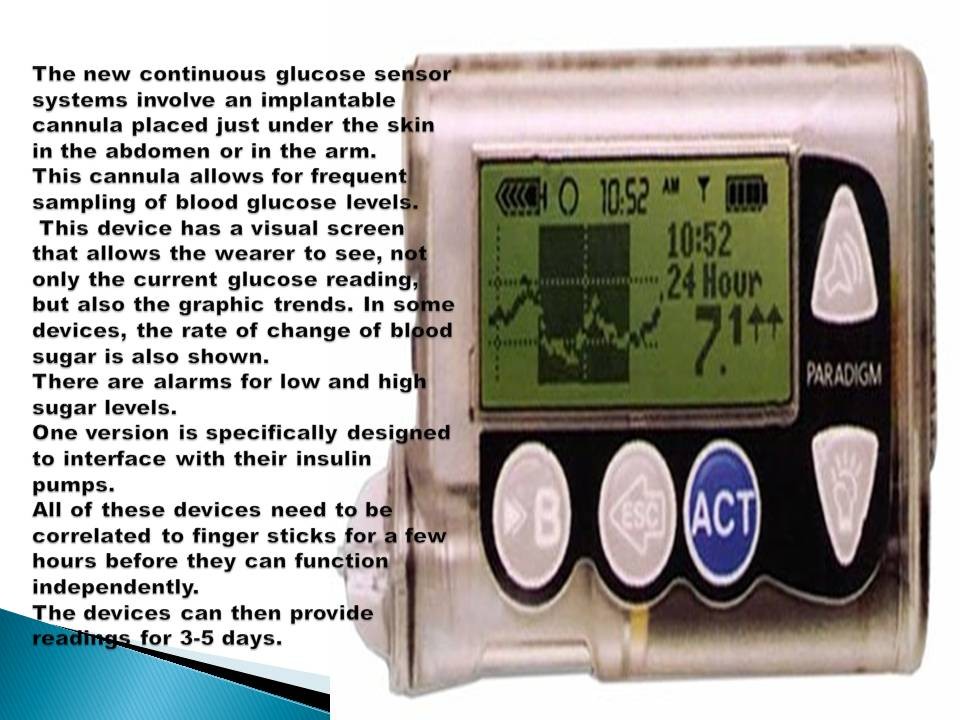
Each meter has its own advantages and disadvantages (some use less blood, some have a larger digital readout, some take a shorter time to give you results, etc). The test results are then used to help patients make adjustments in medications, diets, and physical activities. The new continuous glucose sensor systems involve an implantable cannula placed just under the skin in the abdomen or in the arm. This cannula allows for frequent sampling of blood glucose levels.
This device has a visual screen that allows the wearer to see, not only the current glucose reading, but also the graphic trends. In some devices, the rate of change of blood sugar is also shown. There are alarms for low and high sugar levels. One version is specifically designed to interface with their insulin pumps. All of these devices need to be correlated to finger sticks for a few hours before they can function independently. The devices can then provide readings for 3-5 days. Severely elevated blood sugar levels due to an actual lack of insulin or a relative deficiency of insulin. Abnormally low blood sugar levels due to too much insulin or other glucose-lowering medications. Acute complications of type 2 diabetes in patients with type 2 diabetes, stress, infection, and medications (such as corticosteroids) can also lead to severely elevated blood sugar levels. Accompanied by dehydration, severe blood sugar elevation in patients with type 2 diabetes can lead to an increase in blood osmolality (hyperosmolar state). This condition can worsen and lead to coma (hyperosmolar coma). A hyperosmolar coma usually occurs in elderly patients with type 2 diabetes. Like diabetic ketoacidosis, a hyperosmolar coma is a medical emergency. Immediate treatment with intravenous fluid and insulin is important in reversing the hyperosmolar state. Unlike patients with type 1 diabetes, patients with type 2 diabetes do not generally develop ketoacidosis solely on the basis of their diabetes. Since in general, type 2 diabetes occurs in an older population, concomitant medical conditions are more likely to be present, and these patients may actually be sicker overall. The complication and death rates from hyperosmolar coma is thus higher than in DKA. Hypoglycemia means abnormally low blood sugar (glucose). In patients with diabetes, the most common cause of low blood sugar is excessive use of insulin or other glucose-lowering medications, to lower the blood sugar level in diabetic patients in the presence of a delayed or absent meal. When low blood sugar levels occur because of too much insulin, it is called an insulin reaction. Sometimes, low blood sugar can be the result of an insufficient caloric intake or sudden excessive physical exertion. The actual level of blood sugar at which these symptoms occur varies with each person, but usually it occurs when blood sugars are less than 65 mg/dl. Untreated, severely low blood sugar levels can lead to coma, seizures and in the worse case scenario, irreversible brain death. At this point, the brain is suffering from a lack of sugar, and this usually occurs somewhere around levels of < 40 mg/dl. The treatment of low blood sugar consists of administering a quickly absorbed glucose source.
These include glucose containing drinks, such as orange juice, soft drinks (not sugar-free), or glucose tablets in doses of 15-20 grams at a time (for example, the equivalent of half a glass of juice). Even cake frosting applied inside the cheeks can work in a pinch if patient cooperation is difficult. If the individual becomes unconscious, glucagon can be given by intramuscular injection. Glucagon is a hormone that causes the release of glucose from the liver (for example, it promotes gluconeogenesis). Glucagon can be lifesaving and every patient with diabetes who has a history of hypoglycemia (particularly those on insulin) should have a glucagon kit.
Families and friends of those with diabetes need to be taught how to administer glucagon, since obviously the patients will not be able to do it themselves in an emergency situation.
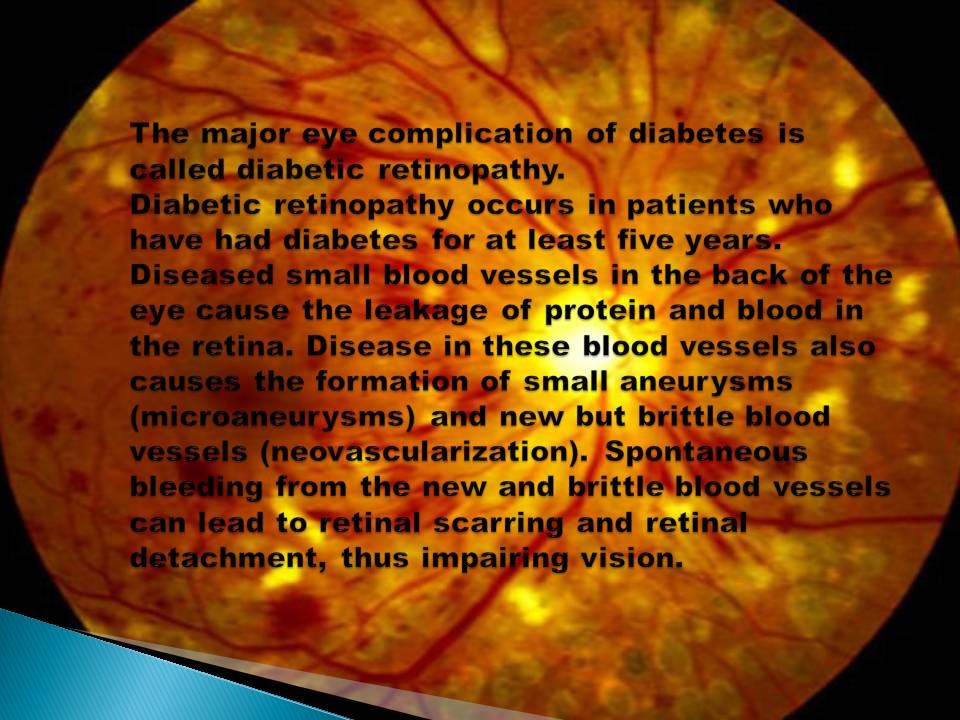
Another lifesaving device that should be mentioned is very simple; a medic alert bracelet should be worn by all patients with diabetes. Diabetic retinopathy to treat diabetic retinopathy a laser is used to destroy and prevent the recurrence of the development of these small aneurysms and brittle blood vessels. Approximately 50% of patients with diabetes will develop some degree of diabetic retinopathy after 10 years of diabetes and 80% of diabetics have retinopathy after 15 years of the disease. Poor control of blood sugar and blood pressure further aggravates eye disease in diabetes. Cataracts and glaucoma are also more common among diabetics.
It is also important to note that since the lens of the eye lets water through, if blood sugar concentrations vary a lot, the lens of the eye will shrink and swell with fluid accordingly.
As a result, blurry vision is very common in poorly controlled diabetes. Patients are usually discouraged from getting a new eyeglass prescription until their blood sugar is controlled.
This allows for a more accurate assessment of what kind of glasses prescription is required. One of the most horror compilations of diabetes is diabetic foot ulcers, which can be difficult to treat and occasionally require amputation. There is no known preventive measure for type 1 diabetes. Type 2 diabetes can often be prevented by a person being a normal body weight and physical exercise.
Diabetic’s medications:
- Metformin is generally recommended as a first line treatment for type 2 diabetes, as there is good evidence that it decreases mortality.
- Routine use of aspirin, however, has not been found to improve outcomes in uncomplicated diabetes.
- Type 1 diabetes is typically treated with a combination of regular and NPH insulin, or synthetic insulin analogs.
- When insulin is used in type 2 diabetes, a long-acting formulation is usually added initially, while continuing oral medications.
- Doses of insulin are then increased to effect.